The results of research conducted by ALIMA (The Alliance for International Medical Action) and our partners on optimising the treatment of malnutrition were published in the British Journal of Nutrition and confirm that the new approach makes it possible to treat more malnourished children, without increasing overall costs and reducing the number of hospitalisations.
Each year, acute malnutrition contributes to half of all child deaths, and yet less than 25% of malnourished children have access to treatment. One reason for this is the overly complex system in place today: malnutrition is arbitrarily divided into two categories: severe and moderate. These categories are managed separately, in different programs, overseen by different actors, and do not use the same protocols and products.
OptiMA aims to break down the treatment barrier that exists between children suffering from moderate acute malnutrition and severe acute malnutrition, by simplifying the admissions criteria for children into malnutrition treatment programs. At the same time, this project includes training caregivers to detect malnutrition at its earliest stage, using a single anthropometric measure for screening, diagnosis and discharge criteria, while reducing the cost of treatment.
OptiMA aims to optimize current protocols in three areas:
1. Earlier detection of malnutrition: Training mothers to use “MUAC” bracelets to regularly measure their child’s Mid-Upper Arm Circumference, in order to detect the first signs of malnutrition.
2. Coherency: Using the “MUAC” bracelet as the only admissions criteria (in addition to oedema) to detect and and increasing the threshold to identify children suffering from wasting as early as possible, to make it easier for health staff to care for them, and easier for families to understand.
3. Simplify treatment: Using a single Ready-to-Use Therapeutic Food (RUTF) at a gradually reduced dosage, as children progress in treatment.
With OptiMA, the diagnosis and treatment of malnutrition can occur earlier, and more than twice as many children can access treatment at a cost similar to the current approach.
The OptiMA study took place in the Yako district of Burkina Faso in 2017, and included 4,958 children. The OptiMA protocol is now being implemented in Niger, Mali and the Democratic of the Congo, and preliminary results from a follow-up study in Burkina Faso are being analysed.
To learn more about the OptiMa Burkina Faso project, read the article and study published in the British Journal of Nutrition: https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/new-approach-to-simplifying-and-optimising-acute-malnutrition-treatment-in-children-aged-659-months-the-optima-singlearm-proofofconcept-trial-in-burkina-faso/C55CBF3177D6C44F8D52B09409B40B2C
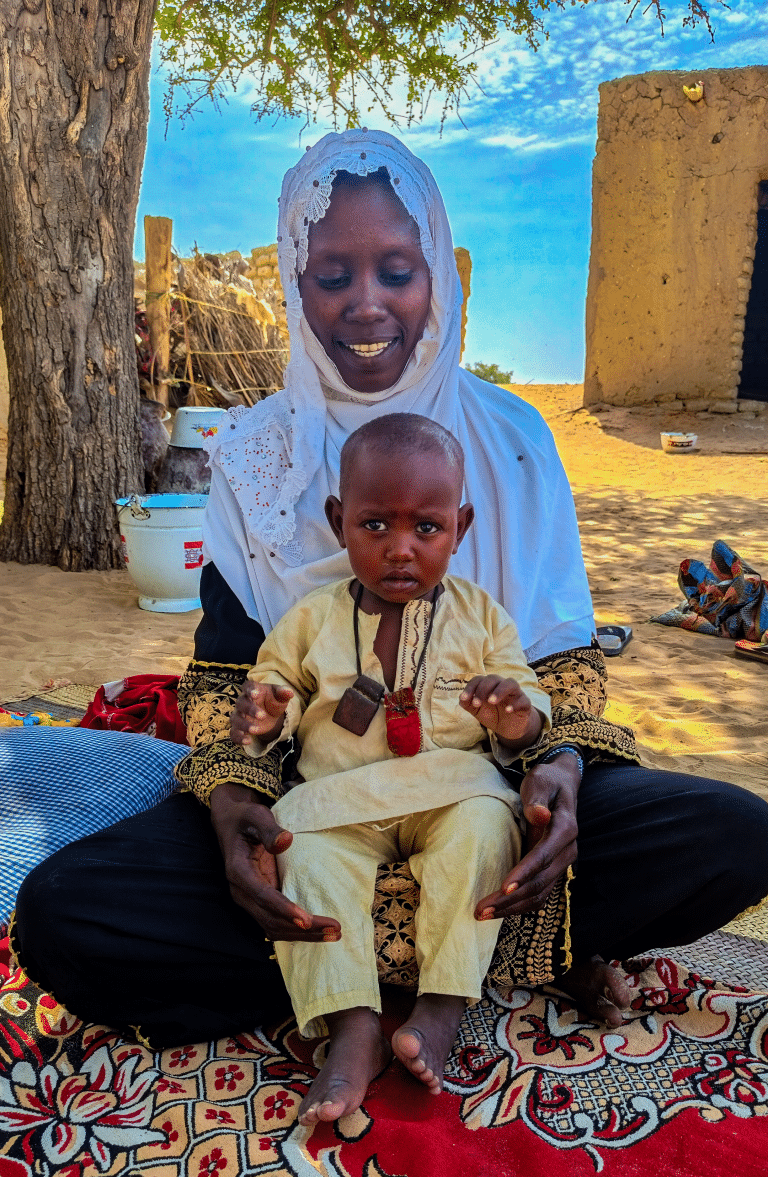
Cover photo: © What Took You So Long? / ALIMA