At 52 years old, you are a renowned surgeon, President of the Nigerien NGO BEFEN (Well-being of Women and Children in Niger), co-founder of a health school and member of ALIMA’s Board of Directors. Tell us more about how you got here.
My passion for medicine goes back to my childhood. Whenever the head of the district medical center would come on a mission to the areas surrounding my village in Niger, my family would host him. I used to bring him his meals, and with time, a certain relationship developed with him and his team. I wanted to become like them; I wanted to be a ‘Major’ [French for ‘senior nurse’], as they used to call all health workers at the time.
After high school, I studied general medicine for 8 years at the University of Niamey, in the capital of Niger. The medical school was located in a very poor neighborhood; its students were very much in demand for home consultations to help the poor. At the end of my 7th year, with a group of classmates, we wanted to do more. A desk and a bed were all it took to open a small kiosk where we offered free consultations. First on weekends, then every evening. And finally we organized rotating sessions to keep the kiosk always open. We were overwhelmed.
I proposed to the group to create an association so that we could make our work sustainable. We were able to get some small grants to buy medicines, mosquito nets, etc. This is how the NGO BEFEN, Well-being of Women and Children in Niger, was created in 2002. Why this name? Because 80% of the people who came for consultations were women and children.
Care for the most vulnerable, maternal and child health, local trainings… Your philosophy fits well with that of ALIMA. Tell us more.
And that’s why our partnership quickly became a natural development. I met one of the founders of ALIMA who was looking for a partner to develop activities to care for malnourished children.
In 2007, there were already more than 300,000 cases of acute malnutrition in Niger, but the health authorities did not recognize it as a public health problem. Thus, in 2009, ALIMA established its first partnership with an African NGO, the foundation of its current model.
Surgical activities have long been part of ALIMA’s response model, but globally, we see very few humanitarian surgery projects. Why is this?
An esteemed American professor, Dr. Paul Farmer, sums up the situation very well: ‘Surgery is the neglected stepchild of global health.’ Whether governments, aid agencies or donors, few support the development of surgery. Why such a lack of interest, when, according to the Global Surgery 2030 study published by The Lancet’s Commission on Global Surgery in 2015, conditions requiring surgical intervention account for approximately 30% of the global burden of disease?
First of all, because setting up projects to support surgery is expensive. Indeed, an operating room must be equipped with specialized medical devices and supplies; it requires electricity and/or oxygen, and highly specialized human resources, etc. This is all the more challenging since it is often thought that the morbidity associated with a lack of surgical care is less or even negligible. The study shows, however, that every year in West Africa alone, almost 19 million cases that would require surgical care go untreated.
But there is a return on investment: many surgical pathologies – obstetrics, traumas… – concern young patients. This lack of care therefore affects a country’s productivity. It is therefore in the interest of governments to sustainably improve their healthcare systems, in particular by collaborating with humanitarian organizations.
Surgery must be valued and given its place in global health. This is why ALIMA has decided to support two surgery projects in Burkina Faso, since the beginning of 2020.
Can you tell us about the surgery project in Kaya, where you currently practice? Why was this project launched there?
The security and migratory context made us immediately think about such a project. Because of the growing insecurity in Burkina Faso, we are facing a massive influx of internally displaced persons, some of whom have suffered atrocities. Hospitals and other health centers are overwhelmed, all the more so since often the medical staff themselves have fled!
ALIMA has therefore come in support of health in general, but also for emergency, war and obstetrical surgery. We launched the project in March 2020, but we faced a major obstacle: the lack of specialized resources. The Global Surgery 2030 study explains that we would need ‘20 doctors in surgery, anesthesia or obstetrics for every 100,000 people by 2030.’ In Kaya, we are just two surgeons: a Burkinabé from the Ministry of Health and myself from ALIMA, for 163,000 inhabitants! And less than 10 specialist surgeons graduate from the University of Ouagadougou in Burkina Faso each year.
We are currently forced to recruit colleagues from the sub-region, but in the long run, our goal is to participate in the training of enough local staff to ensure that the project is managed by Burkinabé personnel.
What are your goals for 2021?
We have already set up a post-op recovery room adjacent to the operating room, a ward for recent post-operations and an intensive care unit. We have also separated men, women and children within the hospital rooms. Until now, they had been mixed together there.
Before the arrival of ALIMA, there were six medical evacuations per day from Kaya or Barsalogho to Ouagadougou, the capital. Since the arrival, two weeks can now go by without any need for an evacuation. The most frequent pathologies are visceral emergencies (acute peritonitis, intestinal occlusions, acute appendicitis, hernias), and trauma (gun or knife wounds, burns and fractures).
In 2021, it will be a question of restructuring: in terms of technical platforms, human resources, medications and supplies. In Kaya, we want to complete the two existing blocks with equipment, as well as a third block reserved for orthopedic traumas, to be able to care for those injured by fighting, who are currently coming in at alarming rates.
Currently, in Kaya, one patient dies every week due to a significant lack of specialized human resources. Post-surgical complications account for half of these deaths. In 2021, we want them to represent less than 10%. To be able to save our patients, we need to recruit specialists in imaging and anesthesia. In Kaya, for example, no one can read scans. A radiologist can come from Ouagadougou to do it, but only once a week. We need to send patients who want readings quickly to private clinics, which are affordable to few people.
For the moment, we are creating a platform with several specialists from the sub-region so that when my colleagues or I are on leave or sick, there is a replacement available quickly. Through the “training and capacity building” component of the project, we want to ensure that the national teams are able to handle surgery and anesthesia in a sustainable manner.
Can you share with us a story that has particularly struck you since the beginning of the project in Kaya, where you are currently working?
I will always remember this woman, whom I nicknamed ‘Miss Kaya.’ She was 29 years old, married and was carrying with her an 18-month-old child. At the end of October 2020, she came to see me for a consultation. She had a huge belly. I thought she had come to the wrong door!
The young woman had already seen many doctors and specialists, as far as Ouagadougou. She was sent home understanding that nothing could be done for her. Her husband sent her back to her parents; she went to marabouts because she thought she was doomed. Finally, her sister brought her to see me at the Kaya Regional Hospital Center. She walked with difficulty and breathed heavily. Embarrassed by her large abdomen, her face was full of worry.
The scans she presented to me concluded that there was a tumor of the mesentery, a fatty membrane that feeds the intestines. Hence the refusal of care by the doctors she had seen up to that point. But when I consulted her, I realized that the mass was mobile, so I had a good chance of being able to remove it. She said to me: “If you do nothing, I’m doomed anyway. So I have nothing to lose.”
The operation, from opening to closing, took only 45 minutes. From her belly I extracted a 20 kg ovarian cyst tumor! Ethically, this young woman watched this huge ball grow for 9 months, suffered a lot from it, and was kept away from her loved ones – all because of a lack of access to surgical skills.
Two weeks after the operation, she came back to the hospital to have her stitches removed. She was in such good shape and so well dressed that I didn’t recognize her! I have been calling her ‘Miss Kaya’ ever since. And every week, I receive thanks from her.
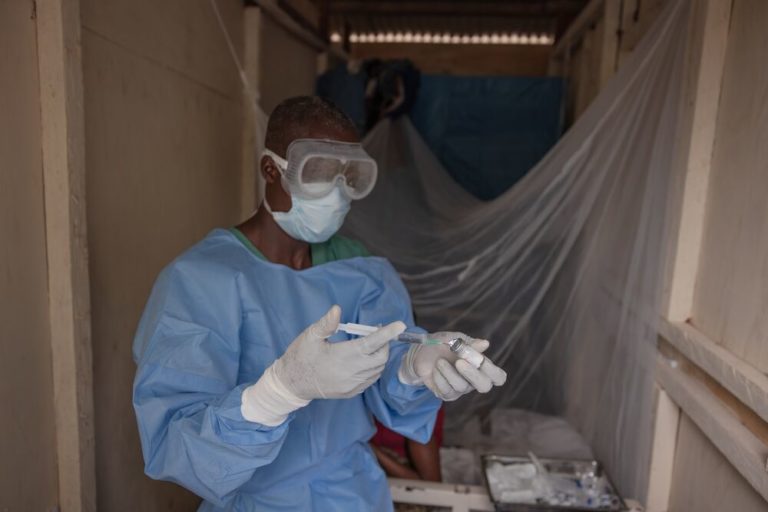
Cover photo: ©️ ALIMA