How did this project come about ?
Dr Maidadji: The project was set up in an area northeast of Tahoua, where health care coverage is very low, where access to medical care is limited by geographical isolation. Only 25% of the population in Tchintabaraden has regular access to health care and 60% of nomadic people live more than 15 kilometers from the nearest health center. The medical needs in this area are therefore enormous.
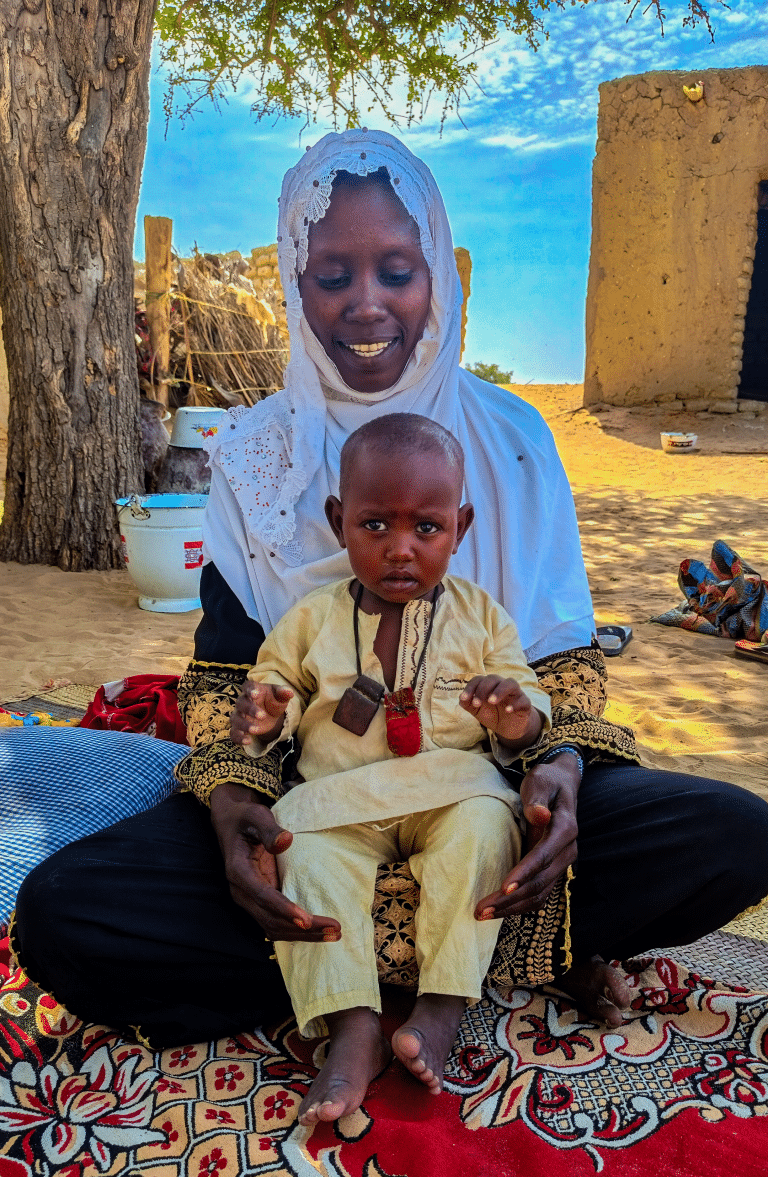
Abankawel Ilitinine: Providing care for nomadic populations is a challenge. With BEFEN/ALIMA, we have been able to put in place a group of health workers who can go to the nomads’ camps to provide the health care they need.
Dr Maidadji: The goal was to work with our partners to help reduce the mortality rate among nomadic populations, with a focus on children under the age of 5 and pregnant women. We thought the best way to do this was to provide a holistic care package that prevents, treats and promotes good health.
We tested some innovative activities. For example, we deployed mobile clinics to areas more than 15km from a health center. We worked with trained liaison officers, who can refer patients to the nearest health center, or provide first aid and dispense medications. Finally, we set up a network of community relays, equipped with telephones that maintain a link between health staff and the nomadic populations who are moving around.
What were the biggest challenges in providing healthcare to nomadic populations?
Dr Maidadji: In some areas, there were problems with telephone reception or availability of electricity to charge the phones. Sometimes there were also linguistic barriers between the health workers and local nomadic groups. Additionally, sometimes people would move to an area that was outside our project’s coverage zone, and so we could no longer provide them with care. But despite all of that, we did our best and even exceeded our targeted goals.
And what impact did this project have?
Dr Maidadji: In partnership with Medecins du Monde Belgium, we supported 12 integrated health centers and 24 community health centers, as well as the district hospital, where ALIMA/BEFEN opened an operating room, as previously, there was no place to perform surgery. We also refurbished medical structures and provided medical supplies and equipment, while reinforcing the capacity of local health agents.
Since the project began, nearly 100,000 children under five received care free of charge and health indicators in the departments of Tilla, Tassara and Tchintabaraden have significantly improved.At the same time, the mortality rate in the pediatrics ward of the Tchintabaraden Hospital decreased from 13.8% in 2015, before the implementation of the project, to 0.74% in 2017.
We helped more than 4,000 women give birth and 10,000 pregnant women received antenatal care. In the surgical block, our teams performed more than 500 ophthalmic surgeries and 700 general surgeries.
Abankawel Ilitinine: During this pilot phase of the project, the results we have seen so far have been very encouraging. It is evident that the model is working, that ALIMA/BEFEN are saving lives. The former model required nomads to travel far distances to receive health care. Today the nomadic populations in Tchintabaraden have access to medical care. This is why we hope that there will be a second phase of this project, and that this model will be integrated into the national health protocol, because, really, it is working.
—–
ALIMA is an international humanitarian medical organization that pools the expertise of aid workers, national medical groups and global researchers to provide high-quality medical care during acute emergencies and recurring crises, throughout 10 countries in West and Central Africa. By sharing resources and know-how, we are increasing at-risk communities’ access to care, while improving humanitarian medicine through research related to malnutrition and disease.
<
ALIMA began its operations in Niger in 2009, where in partnership with BEFEN, teams work to reduce child mortality in Mirriah (Zinder region) and Dakoro (Maradi region) by providing children under five who are suffering from acute malnutrition or other illnesses, free treatment. Since 2014, pregnant women and their children, also benefit from the ‘1,000 Days’ program in Mirriah, in which women receive free health care during pregnancy and childbirth, and then the care extends to their child, up until the age of two. In 2017, in Mirriah and Dakoro, ALIMA/BEFEN cared for more than 42,000 children suffering from severe acute malnutrition, 58,000 patients suffering from malaria, trained 187,000 mothers to use the MUAC and performed 14,000 prenatal consultations.
The “Sante Nomades” (Nomad Health) project was done in partnership with BEFEN, Medecins du Monde Belgium and Niger’s Ministry of Public Health. The project was made possible thanks to funding support from the European Union’s Delegation in Niger.