1. What is Mpox (Monkeypox)?
Mpox, also known as monkeypox, is a zoonosis – an infectious disease transmitted from animals to humans. First detected in humans in 1970 in the Democratic Republic of Congo (DRC), it is caused by a virus belonging to the orthopoxvirus family, similar to the human smallpox virus. Mpox is endemic in certain regions of Central and West Africa, where localised outbreaks are common. While it has predominantly affected Africa in the past, recent cases in other parts of the world have sparked global concern.
2. What Are the Symptoms of Mpox?
Mpox symptoms typically begin with a fever with chills, head and muscle aches, as well as fatigue. Lymphadenopathy (swollen lymph nodes) can also occur, especially in the neck, armpits, and groin. After about two days of fever, a rash appears, usually starting on the face and inside the mouth, then spreading to the torso and limbs (palms of the hands and soles of the feet). The rash progresses from flat spots to raised pimples, then to fluid-filled blisters, and finally to scabs that fall off after two to three weeks. Clinical presentation may vary, and some recent cases have shown skin lesions confined to the genital area without initial symptoms.
3. How is Mpox Transmitted?
Mpox is transmitted through direct contact with the bodily fluids of an infected animal or person, as well as through contaminated objects, such as sheets or clothing. While animal-to-human transmission is more common, human-to-human transmission can also occur, though it is typically less frequent. The virus can spread through respiratory droplets during prolonged close contact, as well as through direct contact with skin lesions or mucous membranes. Sexual transmission is also possible.

4. Who is Most at Risk of Getting Mpox?
People living in endemic areas or in close contact with wildlife are at higher risk of contracting Mpox. Recent outbreaks have also shown a higher prevalence among MSM (men who have sex with men) communities, due to transmission modes involving close and intimate contact. Children and immunocompromised individuals are also more likely to develop severe forms of the disease.
5. What Treatments Are Available for Mpox?
Treatment of Mpox is primarily symptomatic, aimed at relieving symptoms and preventing complications. In most cases, the disease resolves on its own within two to three weeks. Some antiviral medications can be used, although there is limited evidence of their effectiveness against Mpox. If necessary, passive immunisation with specific immunoglobulins may also be considered.
6. What Is the Current Status of Mpox Vaccines?
Two vaccines are currently used to control Mpox, both recommended by the Strategic Advisory Group of Experts on Immunization (SAGE). The WHO recommends these vaccines only for people at risk, such as those who have had close contact with infected individuals or belong to groups particularly exposed to the virus. The organisation does not currently recommend a mass vaccination campaign.
The Africa CDC estimates that around 200,000 doses are available, while the vaccination plans of the affected countries indicate that at least 10 million doses are needed.

7. Why Are the Authorities Concerned About the Mpox Virus?
Global health authorities are concerned about the increasing spread of Mpox beyond its traditional endemic areas, suggesting that the virus may now have an enhanced ability to be transmitted between humans. The current outbreak features concerning aspects, including a new strain, known as “clade Ib”, which appears to be more virulent. This strain is associated with widespread geographic spread and potentially more efficient transmission, including through sexual contact. It also shows a higher impact on children and increased mortality. Additionally, the new strain is associated with various side effects (eye, skin or genital) after recovery. The WHO has declared a Public Health Emergency of International Concern to mobilise the necessary resources to fight this emerging virus.
8. Mpox: What Does the Triggering of the Highest Level of Alert by the WHO Change?
The WHO’s highest level of alert for Mpox reflects the gravity of the situation and the need for a coordinated global response. This means that countries need to enhance surveillance, develop diagnostic capacity, and prepare for a potential rise in cases. This alert also aims to raise awareness among the public and health professionals to prevent a wider spread of the virus.
9. Mpox: What to Do to Avoid a Global Pandemic?
To prevent Mpox from evolving into a global pandemic, early detection of cases, isolation of infected individuals, and close monitoring of their contacts are critical. Vaccination of at-risk populations, along with increased awareness and community-based prevention measures, is also essential. Ongoing research into the virus’s transmission methods and mutations is essential to adapt strategies to control the disease.
10. What Are the Steps to Take if You Think You May Be Infected With Mpox?
If a person thinks they are infected with Mpox, they should immediately self-isolate to avoid spreading the virus. They should seek advice from a healthcare professional for a diagnosis and follow recommended treatment as well as isolation protocols. Close contacts should be notified so that they can be monitored or vaccinated if needed. Maintaining strict hygiene practices, such as frequent hand washing and disinfecting surfaces, is also important to reduce the risk of transmission.
Discover our other articles on this topic
- Mpox Epidemic: What is Alima Doing?
- Report: Fighting the Mpox Virus in the Heart of the Democratic Republic of Congo
ALIMA is at the forefront of the fight against Mpox.
Support our efforts: every donation makes a difference.
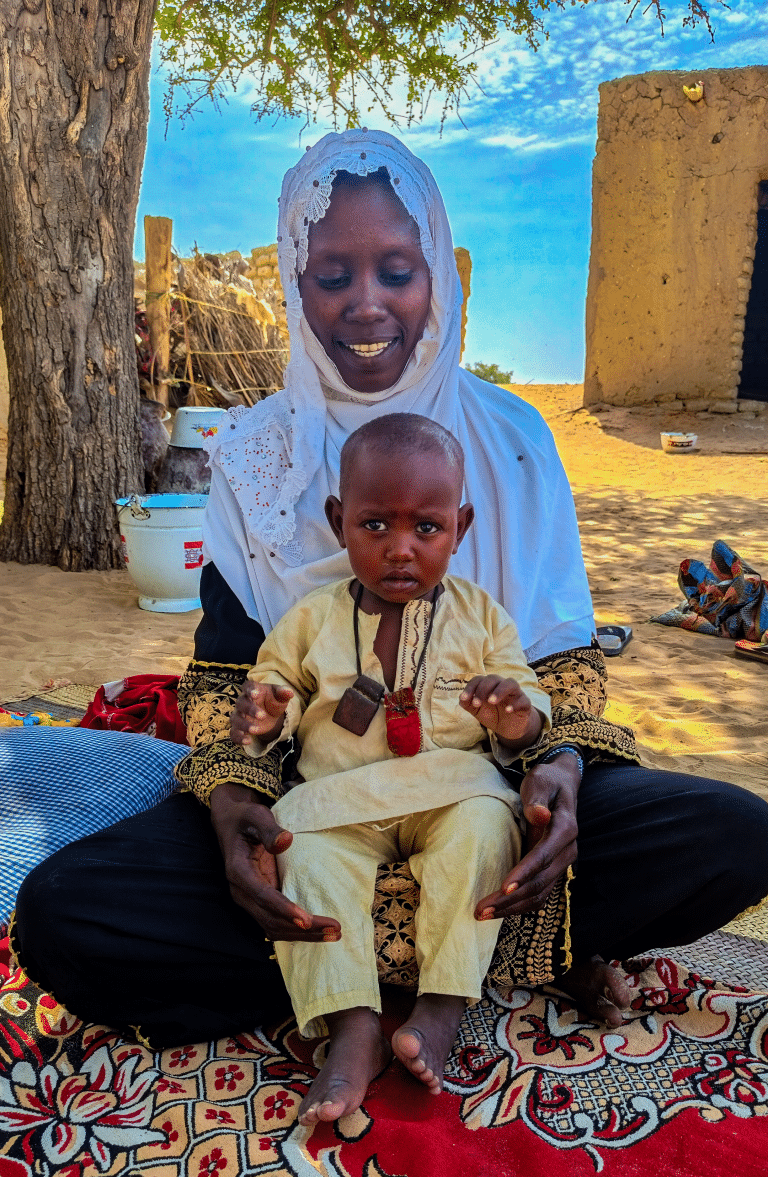
Cover picture © Guerchom Ndebo / ALIMA