“The response and management of this outbreak in DRC is very different from that in Guinea. This time, there is this great innovation that we call the CUBE – a biosecure emergency care unit for outbreaks.The CUBE really changes the way that we, as doctors, can interact with a patient. The time you can spend with a patient is much more than it was in Guinea, because there, when you entered the tents, you always had to go inside wearing the full PPEs (Personal Protective Equipment). It was hot and cumbersome, and you couldn’t stay long.
Can you imagine, each time, putting on and taking off a PPE at every moment? Always, I would need to dress to go inside the tent. I would spend 15, 20 minutes making sure every piece of equipment was properly worn, so that I was protected. Then, you finally go into the tents, but can stay just for a short time. Now, when I need to enter the treatment zone, because of the ventilation system in the CUBE, I can stay longer.
Before, we always had to go inside in teams of two, to support each other. This required many staff. And from the inside, you couldn’t see your colleagues. Here, as I treat a patient, I can talk to other doctors, give them the patient’s’ vital signs and discuss treatment. They can safely guide me from the exterior; they can take notes, which don’t have to be destroyed when I exit; if I need additional equipment or medication, they can pass it to me through the walls of the CUBE.
I can also perform certain procedures from the exterior. In less than a minute, I can put on gloves and can monitor and a patient’s’ vital signs, pass medications, ask them how they are doing; even perform intensive care. This is especially important if there is an emergency…if a patient requires care right away. They can’t wait 15 minutes for a doctor to suit up.
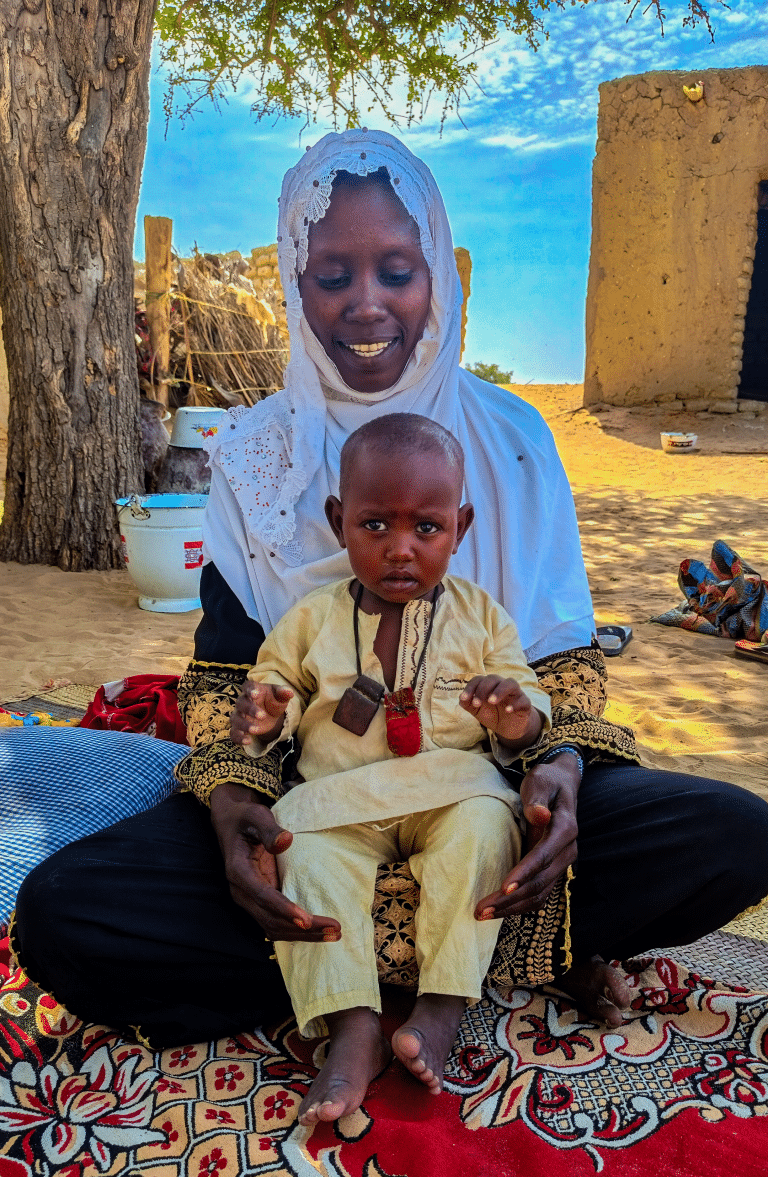
But more importantly, the patients are less stressed, less scared. Before they were terrified to go into the tents; they were terrified to see a masked person. Now they can see our face, they know who we are. And family members can come visit, talk with the patient, see what treatment they are receiving. This was never the case in Guinea, where patients would enter into the tents, and no one from the outside could see in.
Beyond the CUBE, even the tents for suspected cases are an improvement during this outbreak. In Guinea, you could have 20 or 30 or 40 beds within one big tent. Patients next to each other, not knowing who was positive or negative. If a suspected patient tested negative, we could never be certain he or she had no contact with a patient in a neighboring bed who ended up being positive. We tried our best to monitor everyone – the medical team is hyper-vigilant, but the reality was you can turn your back for one second and not know what happens behind you. Here, we are sure suspected patients have no contact with each other because each has his or her own tent.
Of course, there are small things to fix, additional improvements to be made, as this is the first time the CUBE is being used to treat confirmed Ebola patients. We have noticed certain things that could be changed, so it’s still not perfect. But it is an innovation that we, the medical team, really appreciates. It is something that entirely changes our response to Ebola and the manner of treating patients. And with even more lessons learned this time around, the model will continue to improve and the next version will enhance patient care even further. Truly, the CUBE is saving lives.”